Abstract
Background: Early studies reported laboratory changes and hematologic abnormalities in severe cases of COVID-19, although the relation between these findings and the course of the disease is not well established.
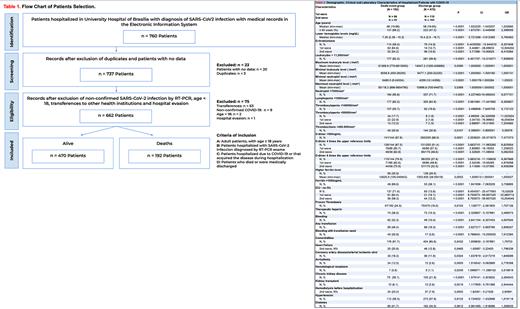
Methods: In this observational, retrospective study we aimed to analyze clinical, biochemical, and hematological findings in hospitalized adult patients with COVID-19 that were admitted in the University Hospital of Brasilia from April 2020 to December 2021.The first (1st) and second (2nd) waves dates were defined in accordance with Johns Hopkins University. Study was approved by the local ethics committee. All records of hospitalized patients with positive RT-PCR for SARS-CoV-2 were analyzed (N=760). A total of 662 were included in this study (table 1). Patients were dived in two groups according to outcome (death or hospital discharge). The analysis plan (table 2) included continuous variables (e.g., age), as well as categorical variables (e.g., intensive care unit (ICU) admission, comorbidities, bleeding, thrombosis, transfusion need, mechanical ventilation (MV) and renal replacement therapy (RRT)). We also analyzed hemoglobin (Hb), leukocyte levels, erythroblastosis, platelet count, coagulation tests, d-dimer (DD) and ferritin. Univariate and multivariate analysis were performed to identify variables that were significantly associated (p<0.05) with outcome.
Results: Study results (table 2) demonstrated a significant association between death outcome and the following variables: age (68 vs 58 years, p<0.001), lower Hb levels (p<0.0001), erythroblastosis (p<0.0001, OR 8.3), leukocytosis (p<0.0001, OR 7.9), lymphopenia (p<0.0001), thrombocytopenia (p<0.0001, OR 5.2), elevated DD (p=0.0001, OR 7.5), transfusion necessity (p<0.0001, OR 3.9) and high ferritin levels (p=0.0002), especially above 1000ng/mL (p<0.0001, OR 3.7). Patients admitted to the ICU were 22.8 and 10 times more likely to die, respectively, in the 1st and 2nd waves. Reduction in the risk of death in ICU patients between waves are probably due to technical improvement and vaccination.
The presence of erythroblastosis was associated with a 12.5- and 6.4-times greater risk of death, respectively, in the 1st and 2nd waves (p<0.0001). The medians of the lowest and highest leukocyte (respectively, p<0.0001, p=0.0395) and neutrophil levels (respectively, p<0.0001, p=0.0369) were significantly higher in the group that died. Thrombocytopenia below 50,000/mm³ increased the risk of death in the 1st and 2nd waves (both with p<0.0001; OR: 16.1 vs 7.2). Thrombocytosis reduced the risk of death by 40%. DD levels 4 or 6 times above the reference limit increased the odds of death by 6.6 times (both with p<0.0001).
Proven arterial and/or venous thrombosis were more common in the group that died (24.5% vs 16%, p=0.0103, OR: 1.7). Likewise, therapeutic heparin was used significantly more in this group (p<0.0001, OR: 3.5), and therapeutic heparin increased the risk of bleeding in the overall population (p=0.0170, OR: 1.7). Bleeding, including those that required transfusion, were significantly more frequent in the group that died (respectively, 32.3% vs 10.4%, p<0.0001, OR: 4.1 and 20.8% vs 3.6%, p<0.0001, OR: 7.0). Transfusion of red blood cells, platelet concentrates (both with p<0.0001), and fresh frozen plasma (p=0.0003) were significantly more frequent in the group that died. Comorbidities were also significantly higher in this group (91.7% vs 85.6%, p=0.0432, OR: 1.8) with emphasis on heart failure (in the 2nd wave, p=0.04, OR: 1.79), previous coronary artery disease/stroke (p=0.0324, OR: 1.6), arrhythmia (p=0.0005, OR: 2.8), chronic liver disease (p=0.0191, OR: 3.4), hematologic neoplasm (p=0.024, OR: 3.5), chronic kidney disease (p<0.0001, OR: 2.3), kidney transplant (p=0.021, OR: 2.5) and pre-hospitalization RRT (2nd wave, p=0.0002, OR 2.9). Prevalence of hypertension, obesity, diabetes, and lung disease was not different between groups. In multivariate analysis, factors significantly associated with death were thrombocytopenia, erythroblastosis, DD greater than 6 times the normal limit, neutrophilia and MV.
Conclusion: Data from this large retrospective single-center study demonstrated that thrombocytopenia, erythroblastosis, DD greater than 6 times the upper reference limits and neutrophilia were predictive factors of in-hospital mortality related to COVID-19.
Disclosures
Sampaio:AstraZeneca: Other: Speaker. Misael:Zodiac: Other: Scientific event. Xavier:Takeda: Other: Speaker, Advisory board, commented articles and scientific event; Janssen: Other: Speaker, Advisory board, PI in clinical trial and scientific event ; Amgen: Other: Speaker.
Author notes
Asterisk with author names denotes non-ASH members.